Bunions
Even though bunions are a common foot deformity, there are misconceptions about them. Many people may unnecessarily suffer the pain of bunions for years before seeking treatment.
What is a Bunion?
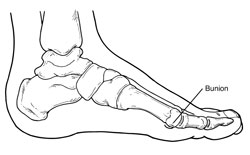
A bunion (also referred to as hallux valgus or hallux abducto valgus) is often described as a bump on the side of the big toe. But a bunion is more than that. The visible bump actually reflects changes in the bony framework of the front part of the foot. The big toe leans toward the second toe, rather than pointing straight ahead. This throws the bones out of alignment – producing the bunion’s “bump.”
Bunions are a progressive disorder. They begin with a leaning of the big toe, gradually changing the angle of the bones over the years and slowly producing the characteristic bump, which becomes increasingly prominent. Symptoms usually appear at later stages, although some people never have symptoms.
Causes
Bunions are most often caused by an inherited faulty mechanical structure of the foot. It is not the bunion itself that is inherited, but certain foot types that make a person prone to developing a bunion.
Although wearing shoes that crowd the toes won’t actually cause bunions, it sometimes makes the deformity get progressively worse. Symptoms may therefore appear sooner.
Symptoms
Symptoms, which occur at the site of the bunion, may include:
- Pain or soreness
- Inflammation and redness
- A burning sensation
- Possible numbness
Symptoms occur most often when wearing shoes that crowd the toes, such as shoes with a tight toe box or high heels. This may explain why women are more likely to have symptoms than men. In addition, spending long periods of time on your feet can aggravate the symptoms of bunions.
Diagnosis
Bunions are readily apparent – the prominence is visible at the base of the big toe or side of the foot. However, to fully evaluate the condition, the foot and ankle surgeon may take x-rays to determine the degree of the deformity and assess the changes that have occurred. Because bunions are progressive, they don’t go away, and will usually get worse over time. But not all cases are alike – some bunions progress more rapidly than others. Once your surgeon has evaluated your bunion, a treatment plan can be developed that is suited to your needs.
Non-Surgical Treatment
Sometimes observation of the bunion is all that’s needed. To reduce the chance of damage to the joint, periodic evaluation and x-rays by your surgeon are advised. In many other cases, however, some type of treatment is needed. Early treatments are aimed at easing the pain of bunions, but they won’t reverse the deformity itself. These include:
- Changes in shoewear. Wearing the right kind of shoes is very important. Choose shoes that have a wide toe box and forgo those with pointed toes or high heels which may aggravate the condition.
- Padding. Pads placed over the area of the bunion can help minimize pain. These can be obtained from your surgeon or purchased at a drug store.
- Activity modifications. Avoid activity that causes bunion pain, including standing for long periods of time.
- Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation.
- Icing. Applying an ice pack several times a day helps reduce inflammation and pain.
- Injection therapy. Although rarely used in bunion treatment, injections of corticosteroids may be useful in treating the inflamed bursa (fluid-filled sac located around a joint) sometimes seen with bunions.
- Orthotic devices. In some cases, custom orthotic devices may be provided by the foot and ankle surgeon.
When Is Surgery Needed?
 If non-surgical treatments fail to relieve bunion pain and when the pain of a bunion interferes with daily activities, it’s time to discuss surgical options with a foot and ankle surgeon. Together you can decide if surgery is best for you. A variety of surgical procedures is available to treat bunions. The procedures are designed to remove the “bump” of bone, correct the changes in the bony structure of the foot, and correct soft tissue changes that may also have occurred. The goal of surgery is the reduction of pain. In selecting the procedure or combination of procedures for your particular case, the foot and ankle surgeon will take into consideration the extent of your deformity based on the x-ray findings, your age, your activity level, and other factors. The length of the recovery period will vary, depending on the procedure or procedures performed.
If non-surgical treatments fail to relieve bunion pain and when the pain of a bunion interferes with daily activities, it’s time to discuss surgical options with a foot and ankle surgeon. Together you can decide if surgery is best for you. A variety of surgical procedures is available to treat bunions. The procedures are designed to remove the “bump” of bone, correct the changes in the bony structure of the foot, and correct soft tissue changes that may also have occurred. The goal of surgery is the reduction of pain. In selecting the procedure or combination of procedures for your particular case, the foot and ankle surgeon will take into consideration the extent of your deformity based on the x-ray findings, your age, your activity level, and other factors. The length of the recovery period will vary, depending on the procedure or procedures performed.
Here are some frequently asked questions (FAQs) and answers about bunions and their treatment.
Are bunions hereditary?
Bunions are most often caused by an inherited faulty mechanic structure of the foot. It is not the bunion itself that is inherited, but certain foot types that make a person prone to developing a bunion.
Do over-the-counter pads and splints really work?
Pads placed over the area of the bunion may help minimize pain from a bunion. However, padding and splinting cannot reverse a bunion deformity.
Will my bunion get worse?
Because bunions are progressive, they don’t go away, and will usually get worse over time. But not all cases are alike. Some bunions progress more rapidly than others.
Is it better to have it fixed now, or should I wait?
When the pain of a bunion interferes with daily activities, it’s time to discuss surgical options with your foot and ankle surgeon. Together you can decide if surgery is best for you.
How can I avoid surgery?
Sometimes observation of the bunion is all that’s needed. A periodic office evaluation and x-ray examination can determine if your bunion deformity is advancing, thereby reducing your chance of irreversible damage to the joint. In many other cases, however, some type of treatment is needed, such as changes in shoes, padding, activity modifications, pain medications, icing, injection therapy, and orthotic devices. When the pain of a bunion interferes with daily activities, it’s time to discuss surgical options with your foot and ankle surgeon. Together you can decide if surgery is best for you.
Will my insurance company pay for the surgery?
In most cases, yes.
Is the surgery painful?
The amount of pain experienced after bunion surgery is different from one person to the next. Most patients will experience discomfort for three to five days. If you closely follow your foot and ankle surgeon’s instructions, you can help minimize pain and swelling after your bunion surgery.
What type of anesthesia is involved?
Most bunion surgeries involve local anesthesia with intravenous sedation. That means your foot will be numb and you will be given medications to relax you during the procedure.
If I need surgery, how long will recovery take?
The length of the recovery period will vary, depending on the procedure or procedures performed. Your foot and ankle surgeon will provide you with detailed information about your recovery.
Will I be able to walk normally, or even exercise and run, after healing from bunion surgery?
In most cases, yes.
How soon can I walk after surgery?
It depends on your bunion and the surgical procedure selected for you.
How soon can I go back to work after surgery?
The length of the recovery period will vary, depending on the procedure or procedures performed.
How soon can I drive after surgery?
The length of the recovery period will vary, depending on the procedure or procedures performed.
Can the bunion come back?
Yes, there is a risk for bunion recurrence in some cases. Patients can help prevent this by following their doctor’s instructions to wear arch supports or orthotics in their shoe.
If screws or plates are implanted in my foot to correct my bunion, will they set off metal detectors?
Not usually. It can depend on the device chosen for your procedure, as well as how sensitive the metal detectors are.
This information is copyrighted by The American College of Foot and Ankle Surgeons.
